A Day in the Life of a GP
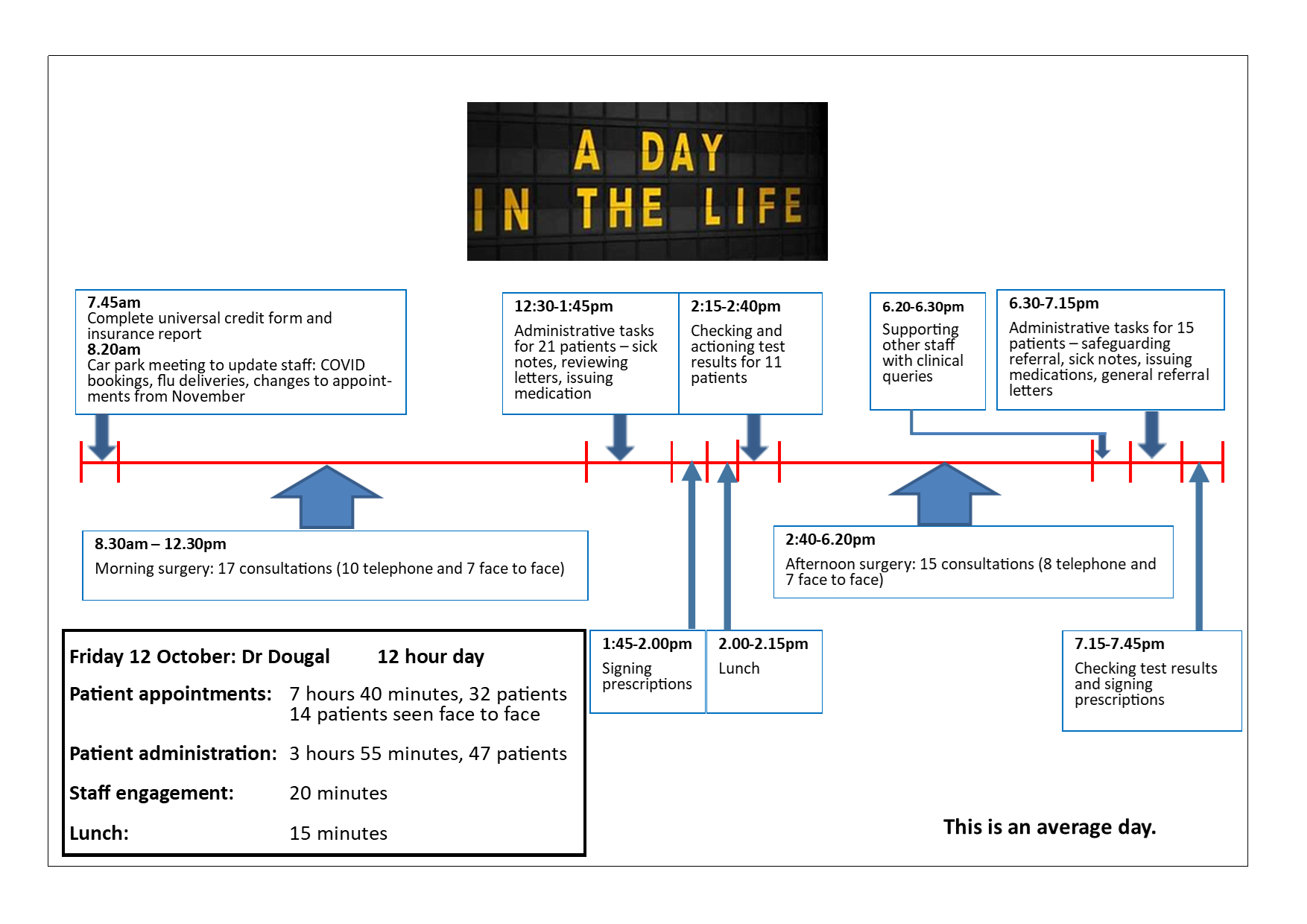
Timeline
Every doctor, nurse and administrative member of the team at Stockbridge Surgery is working hard and doing their best to provide a high standard of care for our patients.
We want the same as you. We also want more doctors and better availability of appointments - unfortunately this is challenging to deliver with the current NHS funding model.
Why are things not what they were 10-15 years ago?
Imagine if Amazon Prime tried to continue with its next day delivery service but was not able to increase the number of delivery drivers to cope with the increasing demand. The result would be it would not be able to offer the same next day service to all its customers as it would not be able to cope with the increased demand when it cannot increase its delivery drivers and factory workers. This analogy is the case for General Practice.
General Practice is funded by what is called a block contract. It is not a payment by activity contract. This means that a GP surgery has a set amount of funding every year based on the number of patients registered with the practice. Whether a patient has 1 appointment in the year or 10 times in the year the funding the practice receives does not change. This means sadly and to our frustration increasing demand cannot be matched with increased staffing. The result is that the more demand on the system, sadly the longer the wait times will be.
This funding model has not changed in the past 20 years - however what has changed is increased life expectancy, increasing complex illness, increasing treatment options for illness, increased awareness and anxiety about illness resulting in desires to see a GP for a problem or symptoms that patients 15 years ago would not book a GP appointment about. There has also been a significant increase in bureaucracy.
We all work in General Practice because we care, and we want to help.
This information, alongside the ‘day in the life of a GP’ timeline has been put together in collaboration with our Patient Participation Group (PPG). Its aim is to be transparent with our patients and to explain the reality on the ground as to why things have changed and sadly why it can feel so difficult to get a GP appointment currently.
Page created: 30 November 2020